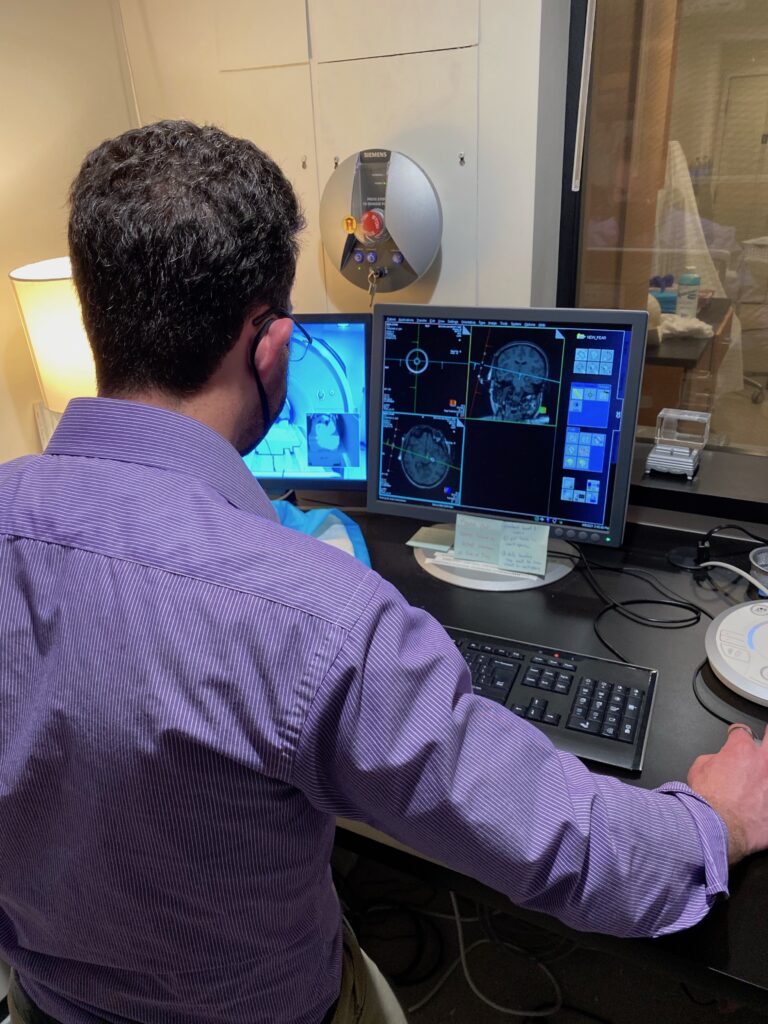
A CfNN Focus Area: Research in Restoring Mental Health employs noninvasive neurotechnologies such as transcranial magnetic stimulation (TMS) and transcranial electrical stimulation (using direct or alternating current; tDCS or tACS, respectively) to understand and change abnormal brain circuit functioning in a group of neurobehavioral disorders that impose health and functional burdens on Veterans, including post-traumatic stress disorder (PTSD), depression, suicide, chronic pain, and obsessive-compulsive disorder (OCD). To map brain circuit function in these conditions we use advanced MRI and electroencephalography methods in collaboration with Neuroimaging and Recording, Decoding, and Computational Neuroscience, with implementation and deployment guided by Assessment, Outcome Measurement, and Implementation.
RESTORING MENTAL HEALTH

Some Mental Health Research Projects:
Research demonstrating that non-invasive brain stimulation, coupled with virtual reality or on its own, can improve PTSD: Research has demonstrated that tDCS, combined with virtual reality exposure, can improve PTSD (van ‘t Wout-Frank et al., 2019); these results led to a Merit-funded study (I01 RX002450) that tested this intervention broadly and with positive results (van ‘t Wout-Frank, Philip et al., 2024). FA-2 also conducted the first randomized controlled study of a novel TMS paradigm (intermittent theta burst) in Veterans with PTSD (Philip et al., 2019). Recent awards of VA equipment grants (IS1 BX004779) an NIMH cooperative study award (U01 MH 123427) support first-in-human testing of low intensity focused ultrasound for depression and anxiety, under FDA IDE G200146.
Precision approaches show that response to TMS can be predicted by specific patterns in brain connectivity: Ongoing work on therapeutic TMS suggests that the antidepressant response to TMS can be predicted by specific patterns in brain connectivity before treatment (Philip et al., 2018; further funded by I01 RX003152). Furthermore, FA2 research demonstrated that data-driven, machine-learning approaches could identify patients most likely to respond to TMS (Zandvakili et al., 2019) and help clinicians determine which patients are most suitable for TMS (Berlow et al., 2019).
Identification of neural circuits underlying risk of suicide: Investigators have identified neural circuits underlying suicide in PTSD (Barredo et al, 2018), and ongoing work is identifying how neuroimaging can identify those at risk for suicide (IK2 CX001824). In collaboration with local health services researchers, we launched the first study to combine brain stimulation and psychotherapy to reduce suicide in high-risk Veterans (I01 HX002572).
Research evaluating the emotional (affective) component of chronic pain: Research evaluating the emotional (affective) component of chronic pain, a clinical feature which magnifies pain-related disability; FA-2 research demonstrated that tDCS can improve pain tolerance (Mariano et al., 2015) and demonstrate improvements in pain-related interference and disability—as well as depression–relative to a placebo condition in a double-blinded RCT (Mariano et al. 2019). Other FA-2 research focused on the use of tACS to modulate pain-related somatosensory perception (Sliva et al., 2018).
Invasive and noninvasive brain stimulation for individuals suffering with intractable OCD and related conditions: FA2 investigators led work resulting in FDA HDE approval of deep brain stimulation (DBS) for intractable OCD (Greenberg, PI), and developed multicenter controlled data showing sustained improvements in functioning after DBS for that illness, which is commonly comorbid with PTSD. Ongoing work has investigated effects of transcranial electrical (tDCS) or magnetic stimulation (TMS) on brain circuits implicated in OCD. Most recently, FA2 investigators and collaborators are characterizing the relationships between OCD-spectrum conditions and interpersonal functioning and quality of life in trauma-exposed Veterans.
Therapeutic transcranial magnetic stimulation is efficacious for PTSD. Work from FA2 and colleagues around VA have reported that therapeutic transcranial magnetic stimulation (TMS) can reduce symptoms of PTSD; in fact, after stimulation 65.3% demonstrated a clinically meaningful reduction in PTSD symptoms, and 46.1% no longer met PTSD criteria (Madore et al., 2022). Furthermore, the team has demonstrated that Veterans with mild traumatic brain injury also respond well to therapeutic TMS at rates that are comparable to those without traumatic brain injuries (Philip et al., 2023).

Noah Philip, MD

Emily Aiken, MA

Samantha Cilli, BS

Amanda Arulpragasam, PhD

Miriam Goldberg, MD, PhD

Jennifer Barredo, PhD
Yosef Berlow, MD, PhD

Erica Eaton, PhD

Mascha (van ’t Wout) Frank, PhD

Benjamin Greenberg, MD, PhD

Timothy Mariano, MD, PhD, MSc

John McGeary, PhD

M. Tracie Shea, PhD

Robert Swift, MD, PhD

Ryan Van Patten, PhD, ABPP